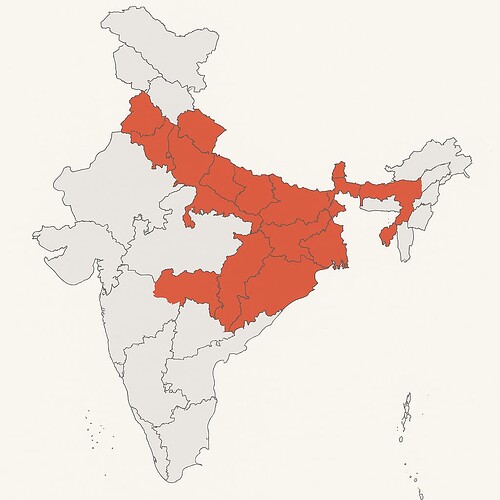
Introduction In India’s vast rural landscape, millions of farming families face a daily challenge beyond their fields: accessing timely healthcare. Despite efforts through public health schemes and infrastructure development, a significant number of villages, especially in states like Uttar Pradesh, Bihar, Jharkhand, Madhya Pradesh, and Odisha, continue to suffer from poor access to healthcare facilities. This report examines the current healthcare availability for farmers in remote villages, highlighting the distances to hospitals, the resulting consequences, and policy gaps that contribute to this critical issue.
1. The State of Rural Health Infrastructure
- According to Rural Health Statistics 2024, India still lacks over 30,000 Primary Health Centres (PHCs) and Sub-Centres based on WHO norms.
- Many existing PHCs operate without doctors, nurses, or basic equipment.
- Only 20% of rural PHCs have functional laboratories or diagnostic tools.
2. Distance from Health Facilities
- Over 40% of villages have no government hospital or clinic within a 5 km radius.
- In tribal and hilly areas, farmers often travel 10–30 km on poor roads to reach the nearest health center.
- In Bihar, more than 1 in 3 villages lack any health sub-centre within walkable range.
3. Transportation and Emergency Risks
- Many villages lack reliable transportation or ambulance services.
- Pregnant women, accident victims, and patients with chronic conditions are at high risk due to delayed care.
- Seasonal floods or broken rural roads worsen access during critical periods.
4. Impact on Farmer Health and Productivity
- Farmers exposed to chemicals (pesticides) often lack access to toxicology or emergency care.
- Delays in treating injuries or illnesses lead to chronic conditions or fatalities.
- Poor health reduces farmer productivity and increases household debt due to out-of-pocket treatment in private facilities.
5. Government Initiatives and Gaps
- Ayushman Bharat aims to offer insurance and Health & Wellness Centres (HWCs), but uptake is low in remote zones.
- Mobile medical vans operate in some states but are inconsistent and under-resourced.
- Health Budget for rural areas remains under 1.5% of GDP – below WHO recommended 2.5%.
6. Regional Inequality in Services
- Kerala, Tamil Nadu, and Himachal Pradesh have made strides in rural health outreach.
- Eastern states like Bihar, Jharkhand, and Chhattisgarh lag behind in both physical infrastructure and human resource deployment.
- Farmers in underserved states face greater medical risk and outmigration due to poor services.
7. Women and Child Health Challenges
- Lack of proximity to hospitals results in home births, maternal deaths, and untreated childhood illnesses.
- Anemia and malnutrition remain high due to absence of regular health check-ups.
8. Digital Divide in Rural Telemedicine
- While telemedicine is promoted, only 25% of rural regions have internet or device access.
- Most farmers are unaware or unable to use digital health services launched under eSanjeevani.
Conclusion Farmers living in India’s villages are not just disconnected from cities but also from critical healthcare. The absence of nearby hospitals and clinics creates a compounding crisis of health and poverty. Without urgent expansion of infrastructure, transport services, and digital access, rural health inequity will persist, undermining national goals of universal health coverage.
Recommendations
- Build PHCs and HWCs in all gram panchayats with >3,000 population.
- Deploy solar-powered mobile clinics in deep-rural areas.
- Create village-level ambulance response hubs through local cooperatives.
- Train rural youth as community health workers with digital toolkits.
- Expand Ayushman Bharat outreach via FPOs and rural banks.
- Incentivize private hospitals to operate satellite clinics in remote zones.
Prepared by: Famalth Research Desk (25 April 2025)